- Treat possible underlying cause if known
- Atropine
- Class 2a treatment
- Dose 0.5 mg IV every 3-5 minutes, up to total dose 3 mg
- Can produce paradoxical worsening bradycardia
- Less effective in patients with cardiac transplant
- Skip if unstable, move directly to pacing
- Transcutaneous pacing
- Class 1a recommendation
- Place pads in anterior lateral or anterior posterior position
- Consider sedation or pain control
- Set monitor to “Pacer”
- Set rate, usually around 60 bpm
- Start current at 0 mA and slowly increase until capture is obtained. Consider different placement of pads if capture not achieved by 130 mA
- Confirm capture by feeling pulse or cardiac ultrasound
- Transcutaneous pacing is ultimately a bridge to transvenous pacing or permanent pacemaker – discuss with cardiology or transfer to center with these capabilities
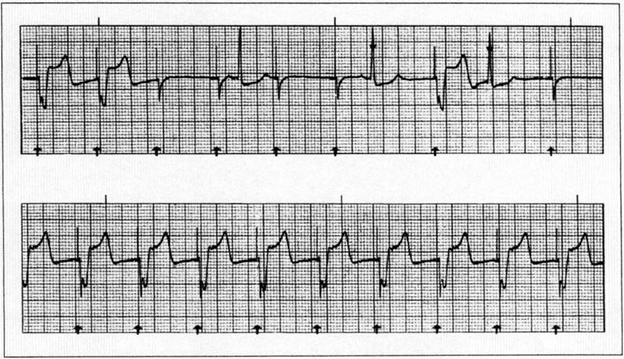
- Capture (pictured below) shows pacer spike followed by a wide QRS and then ST and/or T wave

References:
- Judith E. Tintinall, et al. (2020). Tintinalli’s Emergency Medicine : A Comprehensive Study Guide (Ninth Edition). New York: McGraw-Hill.
- Doukky R, Bargout R, Kelly RF, Calvin JE. Using transcutaneous cardiac pacing to best advantage: How to ensure successful capture and avoid complications. J Crit Illn. 2003 May;18(5):219-225. PMID: 30774278; PMCID: PMC6376978.
- Holger J S, Lamon R P, and Minnigan H J et al.: Use of ultrasound to determine ventricular capture in transcutaneous pacing. Am J Emerg Med. 2003; 21: 227