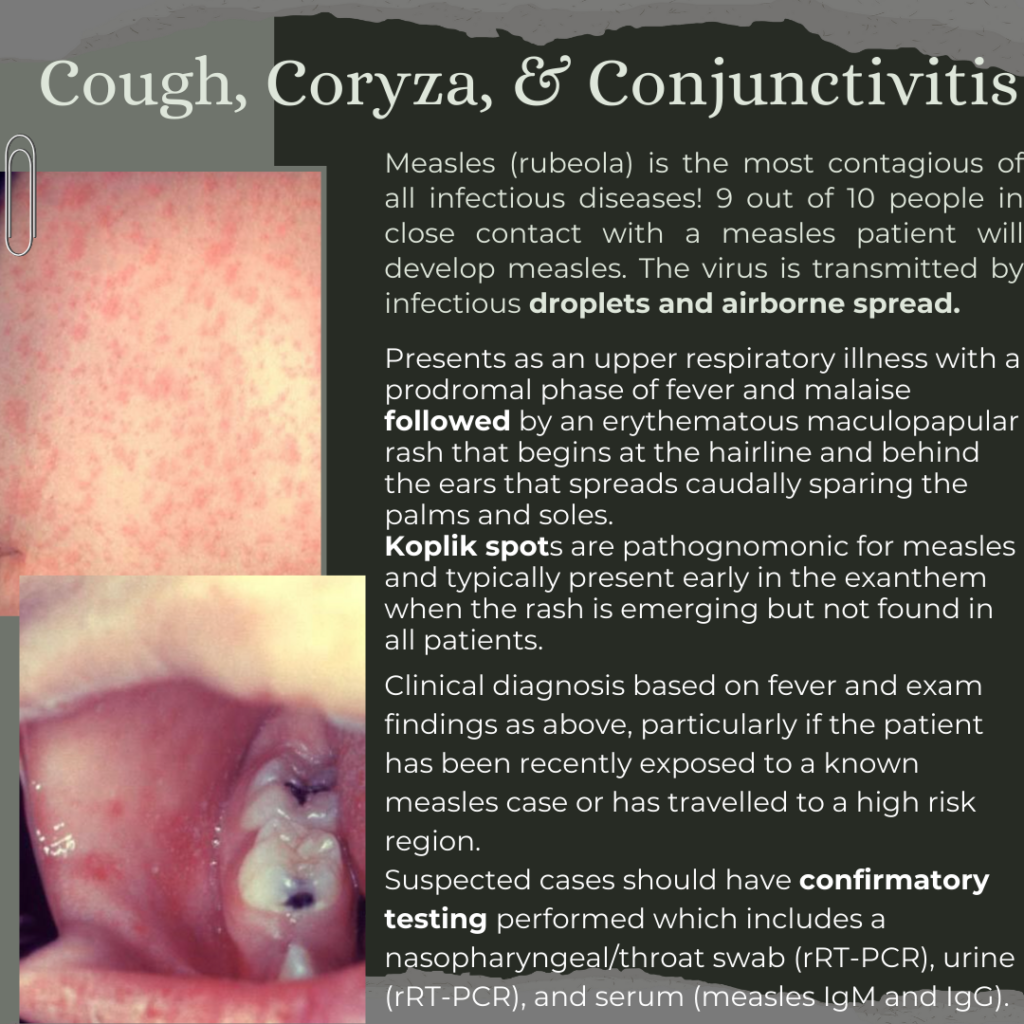
The patient is a 40-year-old male with no past medical history who presents with concerns of a rash on his hands. He states that the lesions appeared two days ago, but had a fever, muscle aches, and pruritis two days before that. He does not have a history of hives or contact dermatitis. He does not take any medications, but states he recently developed “cold sores.” His temperature is 100.6oF, but his other vitals are within normal limits. The cutaneous rash is demonstrated below. When looking in his mouth, blistering lesions are also present. What the diagnosis and management?

Answer: Erythema Multiforme
- Erythema multiforme is the result of a T-cell mediated hypersensitivity reaction resulting in a characteristic pruritic, targetoid papules, with a hazy-center, and surrounding erythematous rings.
- 90% of cases are associated with infectious etiologies, with HSV-1 being most common in adults and Mycoplasma pneumonia in children.
- Remaining 10% are due to drugs (NSAIDs, antiepileptics, antibiotics), malignancy, and autoimmune diseases. Their mechanism of rash formation is unknown.
- There are two specific subtypes:
- Erythema multiforme minor: rash without mucosal involvement or constitutional symptoms
- Erythema multiforme major: rash with mucous membrane involvement and constitutional symptoms (fever, malaise, myalgias etc.)
- Diagnosis is often clinical, but immunofluorescence can be helpful if uncertain.
- PCR testing for both HSV and Mycoplasma pneumoniae should be done if suspected.
- Treatment is mostly symptomatic, and the rash is usually self-limited.
- Antihistamines are useful for pruritis.
- Systemic steroids maybe be used, but the impact on long-term outcomes and symptom duration is unclear.
- Acyclovir may be used to prevent recurrent HSV infections.
- Macrolides may be used in Mycoplasma pneumoniae is suspected.
References:
- Baluzy Matthew, Karaze Tallib. Maculopapular Rashes. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. https://www.emrap.org/corependium/chapter/recvFPlc0BmXxYuzp/Maculopapular-Rashes#h.til8vwjxmfh6. Updated June 21, 2023. Accessed January 24, 2024.
- Sokumbi O, Wetter DA. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol. 2012;51(8):889-902. doi:10.1111/j.1365-4632.2011.05348.x
- Trayes KP, Love G, Studdiford JS. Erythema Multiforme: Recognition and Management. Am Fam Physician. 2019;100(2):82-88.
- J. Brady W, Pandit A, R. Sochor M. Generalized Skin Disorders. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill Education; 2020. Accessed January 24, 2024. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=2353§ionid=221180403
- DermNet. https://dermnetnz.org/topics/erythema-multiforme-images