
Serotonergic Toxicity






Overview:
Local anesthetics are a class of medications that includes esters and amides such as benzocaine/procaine and bupivacaine/lidocaine respectively
Local anesthetics MOA: Primarily through inhibition of voltage-gated sodium channels
Risk Factors for development of LAST:
Clinical Presentation: Primarily affects the CNS and cardiovascular system
CNS: usually presents first
Cardiovascular symptoms:
Treatment:
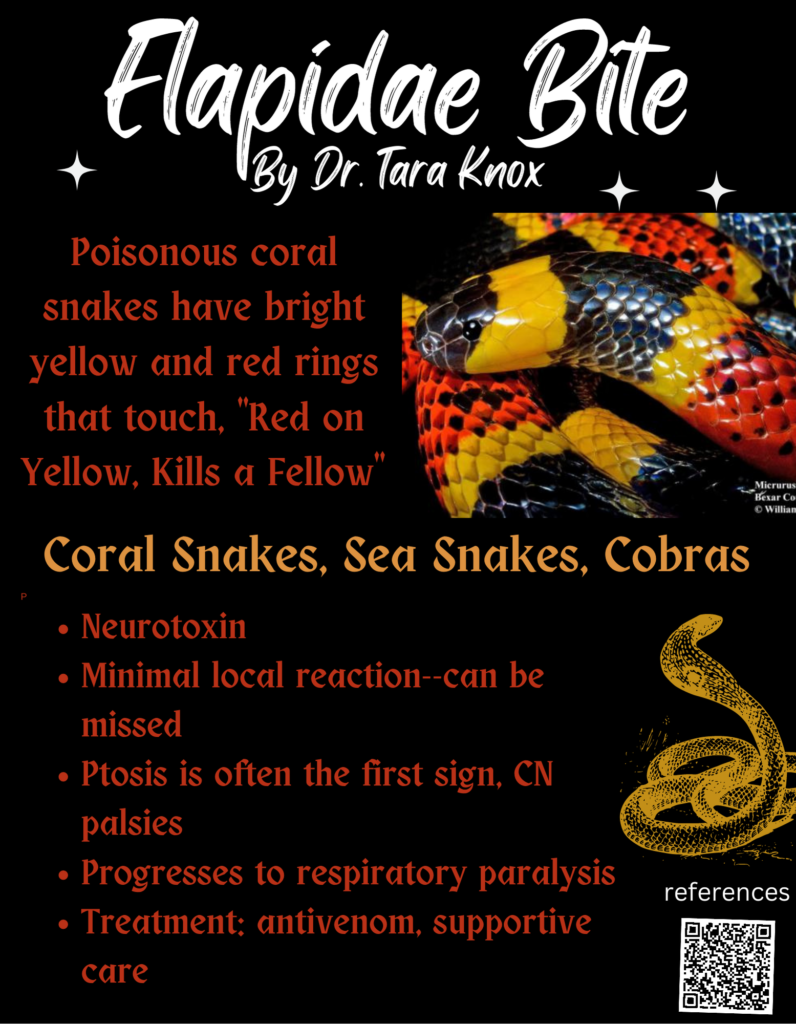

A 24 year old male with no past medical history presents to the ED for a snake bite. He collects snakes as a hobby, and his pet copperhead bit him on his left arm yesterday. Today, he woke up with pain and paresthesias over his left forearm. Vital signs are: Temp 99.8, HR 92, BP 132/90, RR 16, SpO2 98% RA. Exam shows two punctate lesions over the volar aspect of his forearm with mild surrounding erythema and no bleeding or drainage. There is a palpable radial pulse. The forearm is firm and tender to light palpation, and passive flexion of the wrist causes severe pain. 4 mg of IV morphine does not provide any relief. Which of the following is the next best step in management?
A: administer crotalidae polyvalent immune Fab
B: consult general surgery
C: mark surrounding area of erythema and monitor for progression
D: repeat another dose of 4 mg IV morphine
Answer: administer crotalidae polyvalent immune Fab
Compartment syndrome is a rare but known complication of snake bites. The first-line treatment of compartment syndrome in the setting of a snake bite is anti-venom as it is the effect of the venom on tissues that causes elevated compartment pressures. If compartment pressures continue to rise after administration of antivenom, consulting general surgery for a fasciotomy is a last resort intervention. Marking the lead edge of erythema and edema is wise to monitor for progression, but treatment of compartment syndrome should not be delayed. Another dose of IV morphine is not the definitive treatment for this condition.
References:
Dart R.C., & White J (2020). Snakebite. Tintinalli J.E., & Ma O, & Yealy D.M., & Meckler G.D., & Stapczynski J, & Cline D.M., & Thomas S.H.(Eds.), Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill.