A 45 year old male with a history of autism, depression, and epilepsy presents for an overdose. He was found in his bedroom obtunded by family with empty pill bottles. His medication list includes valproic acid and fluoxetine. He was intubated by EMS for airway protection. His vital signs include Temp 98.0F, HR 108, BP 100/60, RR 16, SpO2 99% on 40% FiO2. On exam, he has a GCS of E1 V1T M4 with minimal sedation. Pupils are equal and reactive to light. There is no rigidity or clonus. Labs are notable for elevated LFTs and ammonia. Which of the following medications should be used for the treatment of this patient’s suspected overdose?
A: Cyproheptidine
B: Levo-carnitine
C: Meropenem
D: B & C
Answer: B & C (Levo-carnitine & Meropenem)
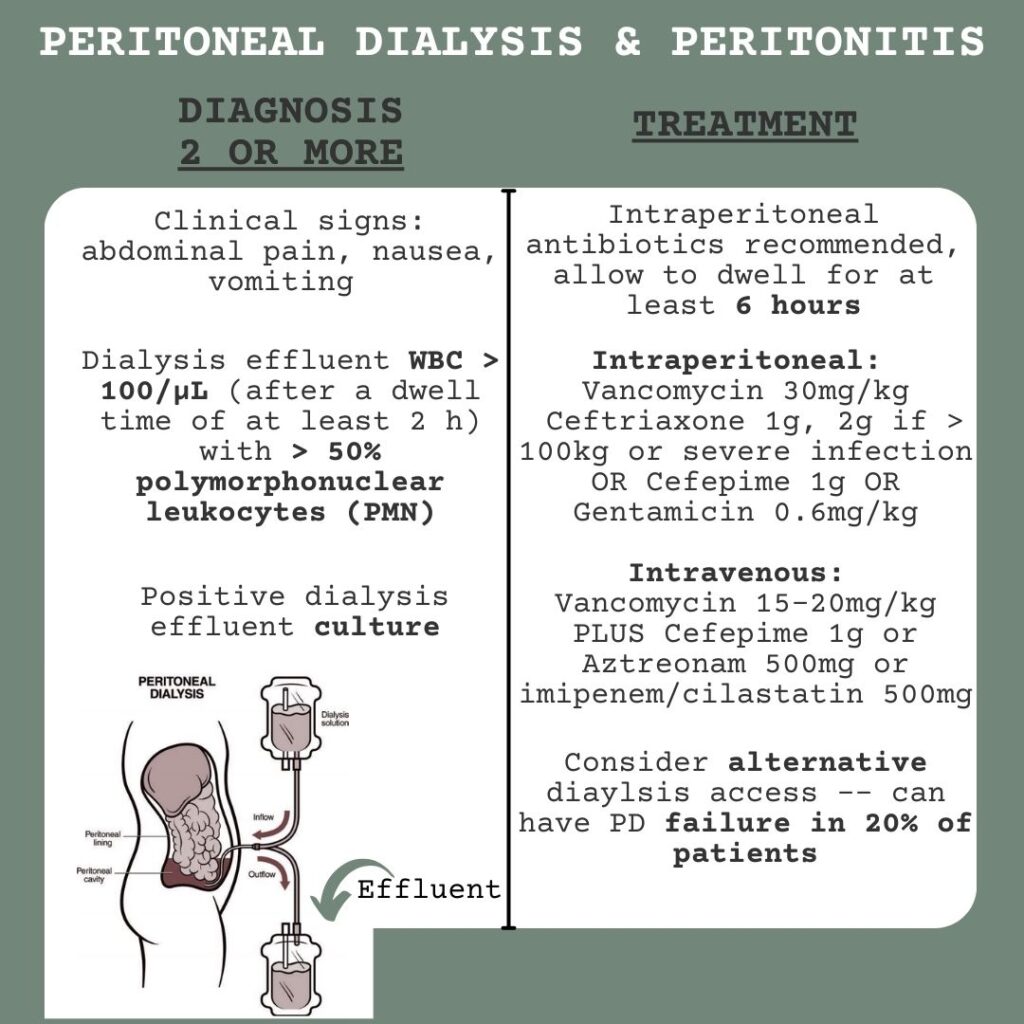
This patient’s presentation is consistent with valproic acid overdose. The most common exam finding is CNS depression which can range from drowsiness to coma. Serotonin syndrome classically presents with hyperthermia and clonus. Treatment of serotonin syndrome typically includes supportive care with benzodiazepines and cyproheptadine with consultation of a toxicologist. Treatment of valproic acid toxicity includes GI decontamination and levo-carnitine as it can increase metabolism of valproic acid, hasten resolution of coma, and prevent hepatic dysfunction. Newer studies have shown that concomitant use of carbapenems (specifically meropenem) with valproic acid causes drug-drug interactions that lead to decreased serum valproic acid concentrations. Dialysis can be considered for severe overdoses with hemodynamic instability or acidosis that does not respond to initial therapy.
References:
LoVecchio F. Anticonvulsants. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill; 2020.
Al-Quteimat O, Laila A. Valproate Interaction With Carbapenems: Review and Recommendations. Hosp Pharm. 2020;55(3):181-187. doi:10.1177/0018578719831974Al-Quteimat, O., & Laila, A. (2020). Valproate Interaction With Carbapenems: Review and Recommendations. Hospital pharmacy, 55(3), 181–187. https://doi.org/10.1177/0018578719831974
Special shoutout to our ED pharmacists that educated us on this topic!